Jump to:
General perimenopause FAQs
What is perimenopause?
Perimenopause is the time during your life before menopause, it’s a natural change that we all go through. Natural menopause doesn’t happen overnight, and the hormonal changes leading up to it can happen over many years.
During perimenopause, progesterone levels initially start to fall which often causes changes to your periods such as heavier or more irregular bleeds. Oestrogen levels fluctuate up and down at the same time while the ovaries are trying hard to release eggs despite there not being many left! Overall, your oestrogen levels slowly drop during the perimenopause.
1 in 4 people won’t get any symptoms at all. However, you may experience a wide range of symptoms including anxiety, brain fog, poor sleep, hot flushes, headaches and symptoms similar to premenstrual syndrome (PMS) which can affect your quality of life.
Perimenopause may last for several years with symptoms coming and going or becoming more and less intense until menopause is reached. You reach menopause when you have not had a period for 12 months.
What's the difference between perimenopause and menopause?
Perimenopause means that you’re going through the changes towards menopause. Menopause is actually only one day in your life — the day when it’s been exactly 12 months since your last period. After this date, you are clinically described as being postmenopausal.
The symptoms felt during perimenopause are due to changes in your hormones. During perimenopause progesterone levels initially fall, which often causes changes to your periods and sleep pattern. As the number of eggs in your ovaries reduces, oestrogen levels fluctuate up and down, sometimes wildly, which can cause symptoms such as hot flushes, headaches and irritability. Your overall oestrogen and progesterone (alongside testosterone) levels gradually decrease until they reach a baseline level at menopause.
After menopause, your baseline hormone levels are lower than during your reproductive years and can cause long-term symptoms such as vaginal dryness and itching, discomfort when urinating, and brain fog. Fun fact — “peri” means “around” in ancient Greek and “post” means “after” in Latin so that’s where these descriptions have come from!
What age does perimenopause start?
Perimenopause can start at different ages but usually begins in your mid-40s. Perimenopause lasts an average of 4 to 8 years before menopause. The average age of menopause in the UK is 51. Symptoms can come on slowly or be quite sudden depending on the changes in your hormones. You can learn more about the symptoms of perimenopause in our blog. Some women may find that their perimenopausal symptoms start as a worsening of premenstrual syndrome or premenstrual dysphoric disorder and the changes are gradual.
It is very important to speak to your GP if you think you may be perimenopausal under the age of 40, especially if you haven’t had a period for 4 months. This is because untreated premature or early menopause can impact your long-term health so an accurate diagnosis is key to getting the right support.
Early menopause may run in some families but, of course, every family is different. Genes may play a role in what age you start perimenopause but it’s not a definite way to predict.
It’s also worth noting that certain medical conditions or treatments can cause perimenopause or menopause early such as autoimmune conditions, genetic conditions such as Turner syndrome or treatment with surgery, chemotherapy or pelvic radiotherapy.
What are the main symptoms of perimenopause?
You will often see it stated that there are 34 symptoms of menopause and perimenopause – but there are more, especially as people describe their symptoms in a variety of ways. You may only experience a couple of symptoms throughout perimenopause or experience every symptom — everyone is different. The average number of symptoms to have is seven, according to a survey by the British Menopause Society.
Symptoms can be caused by the fall in progesterone levels during perimenopause or the fluctuations in oestrogen.
Perimenopause symptoms might include:
- Changes to your periods
- Hot flushes
- Changes to sleep
- Breast pain
- Cyclical headaches
- Palpitations
- Anxiety
- Mood change
- Irritability
- Fatigue
- Skin and hair changes
- Joint and muscular pain
- Genital or urinary symptoms such as vaginal dryness, painful sex and urine infections
- Loss of libido
….but can include more or less than the ones listed above.
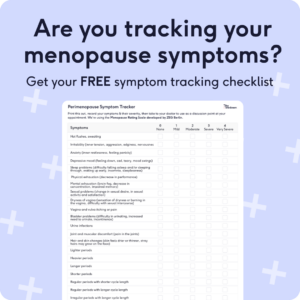
Often, you might start to notice changes in your body that are hard to connect and understand. Keeping a record of all your symptoms, writing them down and taking them to show your GP, can often make it easier to discuss whether these symptoms are due to perimenopause. Our fabulous perimenopause partners at Myla Health have a downloadable perimenopause symptom checker to help make sense of how you are feeling, and they can support you with accessing care and treatment.
How long does perimenopause last?
Perimenopause usually starts between the ages of 40 to 45. Symptoms may only last for a few months or up to 12 years, but the average is between 4 to 8 years. This sounds terrifying, but don’t worry. 1 in 4 of you won’t have any symptoms at all. Symptoms can also come and go throughout this time, with some periods of worse symptoms before they may improve or disappear.
You may wish to speak to any female family members to see how long their symptoms lasted, you may find that your experience is similar to theirs. If you are struggling, there are lifestyle changes and treatment options to support you through this time. Keep reading for the lowdown on this!
Is there a test for perimenopause?
There is a test for perimenopause, but it’s unreliable and the majority of people do not need to be tested.
Over the age of 45, perimenopause should be diagnosed clinically, meaning diagnosis is purely based on your symptoms and does not require any blood tests. A blood test would be unreliable because, during perimenopause, your hormones fluctuate constantly. So a blood test would only show the hormonal levels on that particular day and not the overall picture.
The exceptions to this are if you are under the age of 45 with perimenopausal symptoms, if you are under the age of 40, or if you are on hormonal contraception which stops your periods and want to know if you can stop taking it.
If you are under the age of 40 and have not had a period for 4 months alongside perimenopausal symptoms, you should have a blood test to look for primary ovarian insufficiency (POI) (sometimes called premature ovarian failure or premature menopause). The blood test looks at the level of a hormone called follicular stimulating hormone (FSH) which rises during perimenopause and menopause. Your FSH level is measured twice, 4 to 6 weeks apart, to get an accurate reading and a clear diagnosis. Accurate diagnosis of primary ovarian insufficiency under the age of 40 is important as this can impact your long-term health if untreated and you can access treatment and further support.
Can you get pregnant during perimenopause?
Yes, you can still get pregnant during perimenopause. It may seem unlikely, but your body may still be ovulating (releasing eggs) so fertilisation and pregnancy can still happen. Ovulation may be less frequent and more irregular but while you are still having periods, your body can still release eggs. It is still important that you consider contraception during perimenopause if you want to prevent pregnancy. Contraception can be combined with, or used as part of, hormone replacement therapy (HRT). HRT by itself isn’t a contraceptive! We also have a blog that will help you navigate which contraceptive pill is best during perimenopause.
If you are trying to conceive during perimenopause, there may be fertility support available and it’s worth discussing this with your GP early on or speaking to our experienced fertility nurse specialist.
What are the signs that perimenopause is ending?
Perimenopause symptoms can be variable throughout and may increase and decrease in severity. It’s hard to know whether perimenopause is ending based on symptoms alone. The medical definition of menopause is the day that is 12 months after your last period. This is also the day that perimenopause ends. Therefore the best indication that perimenopause is ending can be your periods.
As the length of time between periods stretches out more and more, it is a suggestion that you’re nearing menopause. Annoyingly, you can go many months without a period then suddenly have one at 10 months, and the 12-month count down to menopause begins again. Still, these large gaps between bleeds suggest perimenopause is ending.
Unfortunately, perimenopausal symptoms may extend after menopause, but it’s difficult to predict which symptoms and who will get them. It’s important to know where to access support if your symptoms are persisting and affect your quality of life. Our partners Myla Health are a great place to start.
Perimenopause symptom FAQs
Does perimenopause cause weight gain?
Weight and perimenopause is complex. Over 50% of people may gain weight during the perimenopause. We understand how frustrating and upsetting it can be when your body changes. It is normal for your waist to become bigger through perimenopause, but you can still maintain your weight. Roughly, people gain around 1.5kg on average each year in perimenopause with a possible weight gain of about 10kg. However, you don’t have to sit back and watch the scales change. Remember that you’re not alone and support for perimenopause weight gain is available, talk to a healthcare professional if you’re feeling concerned.
During perimenopause as oestrogen hormone levels reduce, your body deposits fat around the abdomen, rather than all over the body which is more common when you’re younger. As we get older, our muscle mass decreases which means we burn fewer calories on a day-to-day basis and this can lead to weight gain. Finally, because perimenopausal symptoms can make you feel completely rubbish, you may find that you’re consuming more calories or comfort eating. All in all, perimenopause can be a recipe for weight gain.
However, the biggest predictor of weight gain is still how much you eat and drink, and how much you move. It sounds simple but it’s often really hard to change your lifestyle and lose weight, especially with perimenopausal symptoms. Firstly, get help to control your perimenopause symptoms so you are in a good place to make positive changes. With the right support, it’s possible to make lasting steps to reduce perimenopause weight gain, or lose weight.
Can you be perimenopausal with regular periods?
Yes, you can be perimenopausal with regular periods. Perimenopause often causes changes to periods, but this doesn’t always mean they become irregular. Other changes to your periods such as heavier, lighter, longer or shorter bleeds can occur. Perimenopause has a vast collection of symptoms and is diagnosed on the symptoms you experience.
If you are experiencing symptoms of perimenopause without a change in your periods, you can still be diagnosed with perimenopause! If you’re unsure or confused, speak to your healthcare professional who can discuss a diagnosis in more detail. Taking a perimenopause symptom diary or checker to your appointment, like this one from our partners at Myla Health, can help start the conversation about perimenopause more easily.
Does perimenopause cause headaches?
Perimenopause can cause headaches and this is a very common symptom occurring in up to 90% of us! These headaches are caused by the hormonal fluctuations during perimenopause. Oestrogen levels change a lot around puberty and during perimenopause which is a main trigger for both headaches and migraines.
You may notice a worsening of headaches and migraines around the time of your period, especially as periods can become heavier and longer. Migraines can become more severe during perimenopause; lasting longer and not responding as well to treatment.
Headaches and migraines do tend to improve after your periods have stopped, but it can still take some time for them to resolve completely as your oestrogen levels stop fluctuating, and there may be other contributing factors.
Treatment for headaches and migraines is possible during perimenopause with lifestyle changes, medications and HRT, which when managed correctly can dramatically improve your symptoms.
Does perimenopause cause anxiety?
Yes, perimenopause can cause anxiety. Perimenopause and menopause commonly have an impact on your mental wellbeing due to symptoms such as anxiety, anger, irritability, depression, mood swings and loss of confidence. A survey by the British Menopause Society found that the psychological impact of perimenopause affected the social life of 36% of respondents.
Anxiety may be worse during perimenopause if you have suffered from it before, or may suddenly appear without warning. This all sounds very grim, but identifying that you are suffering from anxiety means you can then access treatment. Treatment is based on your individual circumstances and may involve HRT, antidepressants, cognitive behavioural therapy or meditation techniques.
If the emotional symptoms of perimenopause are affecting your day-to-day life and you are experiencing any thoughts of self-harm or suicide, please please contact your GP, 111 or the Samaritans on 116 123 straight away.
Does perimenopause cause bloating?
Yes, bloating is very common during perimenopause and is usually worse in perimenopause than after menopause itself. Bloating is an uncomfortable or even painful swelling of your abdomen. It can be caused by a build-up of gas, fluid and poo. Some people barely notice their bloating but it can be really distressing for others.
The crazy fluctuations of hormones during perimenopause cause bloating, especially due to oestrogen levels rising before they come crashing down again. Oestrogen causes you to retain fluid which is a major cause of bloating. Other symptoms during perimenopause such as constipation can also cause you to bloat more.
You can take some simple measures to try to reduce bloating including increasing your fluid intake, exercise and reducing the intake of any triggering food or drink. A food diary is a useful tool to identify your triggers by recording when your symptoms are their worst alongside what you have eaten and drunk that day. Common culprits include caffeine, onions, beans and fizzy drinks.
Bloating can be a real nuisance but occasionally can be a sign of other more serious problems. If your bloating is worsening or not improving with the simple treatments above, and you have other symptoms such as a change in your bowel habits like diarrhoea or constipation, problems passing urine, bleeding or pain during sex, you should see your GP for further investigations.
Does perimenopause cause breast pain?
Yes, perimenopause can cause breast pain. Breast pain can come on suddenly due to the erratic hormonal changes during perimenopause, it may be continuous, or it may come and go in relation to your period. You can experience the pain in just one breast, or both, and the pain can be described as tenderness, soreness, burning, stabbing or throbbing. It is often due to increased fluid retention inside the breast tissue.
Breast pain can improve after perimenopause but treatments such as HRT can cause it to continue for longer. Simple treatments like paracetamol, anti-inflammatories and supplements like starflower oil can help improve your breast symptoms.
Does perimenopause cause vaginal dryness?
Vaginal dryness is a very common symptom of perimenopause and affects over 50% over the age of 50. However, we don’t talk about vaginal dryness enough and only a quarter of those affected will actually seek help. Vaginal dryness is caused by reduced levels of oestrogen associated with perimenopause and menopause.
Dryness during sex is one of the first vaginal symptoms you may notice but annoyingly, you can also feel pain and discomfort not just during sex, but in everyday life. Genitourinary syndrome of menopause (GSM) is an umbrella term used to describe a whole spectrum of symptoms that can affect the vulva, vagina and urinary tract leading up to, during, and after menopause — including vaginal dryness.
Vaginal dryness can, confusingly, cause increased vaginal discharge which is more watery and a different colour. Often, people try to treat these symptoms with over-the-counter thrush treatment or may think they have a sexually transmitted infection (STI). Rather than dealing with vaginal dryness alone, speak to your healthcare professional as there are many treatments available including non-hormonal and hormonal products to improve your comfort and help you enjoy sex.
Perimenopause treatment FAQs
What are the treatment options for perimenopause?
Perimenopause can be treated in different ways depending on your symptoms. Lifestyle changes including exercise, diet, sleep and reduction in smoking and alcohol can make a huge difference to your symptoms.
Hormone replacement therapy (HRT) provides your body with the oestrogen that is declining during perimenopause alongside progesterone to protect your womb lining from overgrowing (if you have a womb) in response to oestrogen therapy. HRT can treat many of the symptoms of perimenopause but needs a prescription from your healthcare professional as HRT has some small risks you should be aware of.
Other prescription medications including antidepressants and medications for hot flushes may also be available from your GP if you do not want, or cannot have, HRT. Many supplements or natural remedies can help with symptoms such as poor sleep, fatigue, breast pain and some hot flushes. Complementary therapies and talking therapies such as mindfulness, cognitive behavioural therapy (CBT) and acupuncture may also help manage symptoms.
What types of HRT can be used for perimenopause?
The type of HRT used for perimenopause depends on your medical history and your periods. Everyone takes oestrogen to treat HRT symptoms, and if you have a womb, you will also need to use progesterone to protect your womb lining from overgrowing in response to the oestrogen you’re taking.
If you are still having periods, you will be advised to use cyclical (also called sequential) HRT where you take the progesterone part of HRT for 10 to 14 days each month causing your body to have a monthly bleed at the end of each course of progesterone. Some may only take the progesterone part every 3 months, meaning they only have a bleed every 3 months but this should be done under the guidance of an experienced menopause practitioner.
If you are not having periods, for example, if you use hormonal contraception or have had a hysterectomy, you can use continuous HRT where you take the same HRT every day. This means your hormone levels remain the same throughout the month and you should not have a monthly bleed.
HRT can come in various forms such as tablets, patches, gels or sprays. Oestrogen given via the skin as a patch, spray or gel does not increase the risk of blood clots (which is slightly increased when oestrogen HRT is taken as a tablet). Progesterone can be similarly given as a tablet, patch, vaginal pessary or in the form of a hormonal coil such as the Mirena coil. All of these options are available during perimenopause but treatment is individualised to you, so be sure to discuss your options with your healthcare professional.
The above information is based on UK guidance.
What supplements can help with perimenopause symptoms?
There are many many supplements available for perimenopausal symptoms and we know that 80% of people have tried supplements throughout perimenopause and menopause. Popular choices include isoflavones or phytoestrogens (such as soya products and red clover), St John’s Wort, valerian, black cohosh, evening primrose oil or sage.
Research shows all of these may improve symptoms like hot flushes for some, but the evidence isn’t brilliant, and actually, placebo tablets can have the same effect. It is really important to speak to a pharmacist before taking supplements if you are on any other medications because although supplements seem very safe and ‘natural’, they can interact with certain medications. If you have had breast cancer in the past, please discuss supplements with your oncologist or GP before taking them.
The British Menopause Society recommends that you check your supplements for the THR™ logo, which ensures they have been manufactured to a high quality and with safe doses.
What is the best contraceptive pill for perimenopause?
During perimenopause, you can choose to take whichever contraceptive pill suits you as long as your medical history allows.
The progestogen-only pill can be used alongside HRT for contraception. Some menopause specialists may even use two desogestrel-based progestogen-only pills as part of HRT, but this should only be done on specialist advice.
The combined pill contains both oestrogen and progestogen so can be useful to treat perimenopausal symptoms. The combined pill can be used up until the age of 50 if your medical history doesn’t change and you are eligible to use it. You cannot use the combined pill alongside HRT.
The standard combined pills contain a synthetic oestrogen which is different to the oestrogen used in HRT. Some newer brands of combined pill such as Zoely and Qlaira use a body-identical oestrogen similar to those used in HRT so may be more beneficial for perimenopausal symptoms, but there is no research evidence to support this……yet.
Tags
- Women’s Health Concern Menopause Support Booklet
- Women’s Health Concern Menopause Factsheet
- Menopause, NHS UK
- Menopause, NHS Inform Scotland
- Women’s Health Concern Weight Gain and Menopause Factsheet
- Women’s Health Concern Migraine and HRT Factsheet
- British Menopause Society Nation Survey Infographic
- Menopause and Bloating, On Stella
- Women’s Health Concern Vaginal Dryness Factsheet
- Women’s Health Concern Complementary Therapies Factsheet
- De Franciscis P, Colacurci N, Riemma G, Conte A, Pittana E, Guida M, Schiattarella A. A Nutraceutical Approach to Menopausal Complaints. Medicina (Kaunas). 2019 Aug 28;55(9):544. doi: 10.3390/medicina55090544.
- Elkind-Hirsch K. Effect of dietary phytoestrogens on hot flushes: Can soy-based proteins substitute for traditional estrogen replacement therapy? Menopause. 2001;8:154–156. doi: 10.1097/00042192-200105000-00003
One of The Lowdown’s fab Clinical Directors, Dr Frances Yarlett MBBCh (Hons) BSc (Hons) MRCP (2016) MRCGP DFSRH completed her medical training from Cardiff University in 2013. She is currently working as a salaried GP partner in Sheffield with an interest in complex medical patients and women’s health. Fran is really passionate about patient choice and wants to empower women to take control of their bodies and contraception needs.