Jump to:
General Endometriosis FAQs
What is endometriosis?
Endometriosis is a common health condition, which affects 1 in 10 women of child bearing age. That’s 1.5 million people in the UK and 190 million worldwide.
In endometriosis, cells similar to those usually found in the lining of the womb, grow in other parts of the body. These are called “endometrial deposits” and they can be found on the ovaries, bladder, bowels, pelvic and abdominal walls and in rare cases, even places like the lining of the lung.
As your body moves through its natural menstrual cycle, the womb lining thickens to create a nice home for a potential fertilised egg, before shedding and bleeding if no pregnancy occurs.
The symptoms of endometriosis are caused by these endometrial cell deposits outside the womb responding to your menstrual cycle in the same way – thickening and then bleeding.
As this occurs in places where there is less space for the cells to thicken, and nowhere for blood to escape, this causes pain, chronic inflammation and scar tissue (also known as adhesions). This contributes to the wide range of symptoms people with endometriosis may suffer from.
What causes endometriosis?
There is no easy answer for what causes endometriosis. It is very frustrating for every endometriosis sufferer and those of us who treat it….that we don’t exactly know how, or why the condition happens. There are theories, but nothing has been scientifically proven.
One theory called “Retrograde Menstruation” suggests that during a period some of the womb lining travels the wrong way up the fallopian tubes and ends up depositing in the pelvis or abdomen.
Another called “Metaplasia” suggests that some cells in the body are able to change to cells found in the womb lining in response to inflammation or certain toxins.
We have seen some research that shows endometriosis can run in families and there could be a genetic factor. However, none of these have been proven and the real cause could perhaps be a combination of many different ideas. At The Lowdown, we’re hoping science can help us out and finally come up with an answer!
When does endometriosis usually occur, and can you get it at an older age?
Endometriosis affects 1 in 10, which is a staggering 190 million women and those assigned female at birth worldwide. However, it’s really difficult to understand more about when people present with symptoms or “get” endometriosis. This is firstly, because symptoms can vary so much. Some people get very severe symptoms with minimal endometrial deposits and others get almost no symptoms with widespread endometriosis….and we don’t know why. Secondly, because it takes an average of 7.5 years of symptoms before a diagnosis, we often can’t pinpoint when the endometrial deposits first started to appear. What we do know is that endometriosis can present at all ages from when you start your periods and in some, can continue until the menopause.
What are the main symptoms of endometriosis?
There are up to 20 symptoms of endometriosis. The symptoms are really variable for each person, and not necessarily related to how severe or how many endometrial deposits there are. Symptoms can also be very vague and overlap with other common problems such as IBS (irritable bowel syndrome) or pelvic infections.
The signs that to look out for include the following:
- Painful periods which start from 1 to 2 days before bleeding and continue throughout the bleed. The pain can often be debilitating, meaning women miss school, university or work regularly during their period
- Heavy periods, long periods, spotting in between periods or losing old, dark blood before your period starts
- Pain deep within your pelvis or abdomen during sex or internal medical examinations
- Pain or bleeding when going to the toilet (bladder or bowels) while on your period
- Difficulty getting pregnant. Although it is important to remember that 70% of women with endometriosis fall pregnant naturally
- Fatigue, lethargy and mood changes which are understandable when you read through the symptoms above!
How is endometriosis diagnosed?
The average time it takes for a woman to receive a definitive diagnosis of endometriosis is 7.5 years from when symptoms begin. We completely understand this leaves women feeling fed up, exhausted and perhaps even losing trust with the healthcare system.
The length of time it takes to diagnose endometriosis could be partly due to the symptoms, which can be vague and similar to other common conditions, but also because there is no simple test.
Imaging techniques such as an MRI scan or ultrasound of the pelvis can sometimes show endometriosis, but they are currently not perfect. A gynaecologist called Mathew Leonardi has our full respect for developing an advanced ultrasound technique which can accurately diagnose and stage endometriosis alongside helping to plan surgical treatment, however, very few people are trained in this technique at the moment, but we’re hoping it is more accessible soon.
The “gold standard” for diagnosing endometriosis is via a laparoscopy. This is a small key hole operation in which a camera is inserted into the abdomen and pelvis to look for endometrial deposits. If these are found, they may be treated at the same time.
However, this procedure does involve risks. You will require a general anaesthetic and abdominal surgery is invasive with risks including pain, infection, bleeding and damage to organs such as the bladder or bowel walls. Most women are so fed up with their symptoms they are happy to take these risks for a diagnosis, other women prefer to try treatment options first. This is a personal decision, and I’d advise you to discuss the advantages and disadvantages of both options with your doctor.
There is ongoing research into potential biomarkers (such as blood tests or urine tests) that can be used to make a diagnosis instead of surgery, but that won’t be seen in reality for several more years.
How do I speak to a doctor about endometriosis?
This is a really frustrating time, and we know that those who suffer with awful periods often have to see their doctor multiple times before starting investigations. Concentrate on how your symptoms are impacting your life. If you are unable to work, or do your normal daily activities during your periods, especially if simple painkillers like paracetamol and ibuprofen don’t help, then this really signifies a problem. We have a blog on how to discuss endometriosis pain and how it feels with your doctor. Use this as a framework to start a discussion with your doctor, and state “I am worried that I have endometriosis” so your doctor knows how they can use their time to help you.
Can you get pregnant with endometriosis?
Yes, you can get pregnant with endometriosis! Endometriosis can affect fertility and it also depends on the severity of your condition. Of couples trying to conceive naturally most (60 to 70%) will get pregnant within 1 year of trying, compared to 84% of couples where endometriosis is not an issue. 75% of people with mild endometriosis will conceive within 1 year. 50% of people with moderate endometriosis and 25% with severe endometriosis will conceive within one year of trying.
Use our handy fertility quiz to help you understand more about how to optimise your fertility.
If you have a known condition that could cause fertility problems such as endometriosis, you can often be referred to specialist fertility services sooner than waiting for one year of trying. Speak to your doctor who can advise you further and explain what services are available to you locally.
What is the difference between adenomyosis and endometriosis?
Adenomyosis is where the tissue from the lining of the womb grows into the muscle around the womb. Endometriosis is where tissue from the lining of the womb is found outside the womb. Both conditions can cause very painful and heavy periods. Both conditions can be found alone, or together in the same person. They are often lumped together as one, but they are distinct conditions with different causes and treatments.
Where does the blood go when endo tissue starts bleeding during my period?
When endometrial tissue in the pelvic cavity bleeds during the monthly cycle, it can’t leave your body through your vagina, like a normal period would. This tissue and blood can develop into cysts on the ovaries called an endometrioma, also known as a chocolate cyst. In other parts of the pelvis, the blood causes inflammation in the surrounding areas as it is reabsorbed which can cause a build up of scar tissue and pelvic pain.
Where can endometriosis occur and where does it occur in most cases?
The overwhelming majority of endometrial deposits are found in the pelvis, with most being on the ovaries followed by the fallopian tubes and ligaments which hold up the womb. Superficial endometrial deposits are often found on the lining of the pelvic cavity which is called the peritoneum. It is less common for endometrial deposits to be found on the bowel and vagina, and it is very rare for endometriosis to be found outside the pelvis, for example, in the chest.
What’s the difference between dark and light endometriosis tissue?
Endometrial tissue can have various appearances. They have been described as red, white, clear or black like “powder-burns” or “gunshot” marks. There is no difference between these tissues, it is just how endometriosis shows up in each individual. The skill and experience of your clinician will determine how easily they can identify the different types of tissue by sight. Sometimes, taking a small biopsy may be useful to look at the tissues under a microscope to confirm endometriosis.
Is there ongoing research or promising developments in the treatment of endometriosis?
Yes! Menstrual disorders are named in the UK Government’s Women’s Health Strategy as a priority area to improve care and the World Health Organisation are “partnering with multiple stakeholders, including academic institutions, non-state actors and other organizations that are actively involved in research to identify effective models of endometriosis prevention, diagnosis, treatment, and care”. This hopefully means continued investment into research and more support for those who suffer from endometriosis. One of the most exciting areas of research is into diagnosis of endometriosis. As we know, a formal diagnosis often requires invasive surgery, which is not ideal. Research into specific bio markers like blood tests and urine tests to diagnose endometriosis is ongoing. The development of advanced ultrasound techniques is really exciting. Professionals who can use the advanced technique are more able to diagnose endometriosis on ultrasound alone and we hope more practitioners can access this high quality training soon so it is available worldwide.
Endometriosis symptom FAQs
What does endometriosis pain feel like?
Endometriosis pain may be felt as burning, stabbing, pressure-like, cramping, throbbing or any other description of pain found in a thesaurus. Pain is subjective meaning people feel it in individual ways. We have collected descriptions about how other people describe endometriosis pain and how to speak to your doctor about endometriosis pain in our blog.
Can endometriosis cause infertility?
If endometriosis is left untreated, it can cause infertility in some sufferers. However, we still don’t fully understand how it all works. Endometrial deposits can cause adhesions (scar tissue) where pelvic organs become stuck together through inflammation which may affect ovulation or the movement of the egg. Endometriosis on the ovary can cause cysts called endometriomas which can also affect the ability to get pregnant. Learn more about endometriosis and fertility in our deep dive blog.
Up to 50% of women who are being investigated in fertility clinics are found to have endometriosis, and for many of them struggling to get pregnant is their only symptom.
Just because you have a diagnosis of endometriosis does NOT mean you can’t conceive naturally. We do know that most couples (60 to 70%) will get pregnant within 1 year of trying to conceive, compared to 84% of couples where endometriosis is not an issue.
FYI, our CEO Alice has endometriosis and conceived her first baby naturally after an ectopic pregnancy, you can follow her story here.
Does endometriosis affect the development of a child during pregnancy?
Endometriosis can have a small increased risk of miscarriage in the 1st trimester of a pregnancy. Those with endometriosis can also have an increased risk of an ectopic pregnancy compared to women without endometriosis.
Endometriosis does not affect the development of a child, but may increase the risk of complications during pregnancy (such as gestational diabetes, high blood pressure, placenta praevia and preterm labour). However, the research into these complications is of low quality so can’t be relied upon and guidelines don’t suggest that anyone pregnant with endometriosis needs additional monitoring.
Can endometriosis cause weight gain?
Endometriosis can cause some women to gain weight, but the causes are complex and there is little research into the association between weight and endometriosis.
Endometriosis itself can cause bloating and water retention can look like weight gain on the scales. Not only this, but also treatments for endometriosis such as hormonal treatment may cause fluid retention, bloating and in some women weight gain.
Endometriosis affects all aspects of your life, and with chronic pain, it may become harder to exercise and make healthier food choices (we all know chocolate and carbs are quick fixes for those low moments). Therefore, weight gain could be a by-product of living with a chronic condition. However, don’t worry, with effective treatment of your symptoms and addressing lifestyle changes, you can find a balance which allows you to maintain a steady weight. Our pelvic health physio Kathryn is also an endometriosis coach and a perfect person to speak to for motivation and support with these lifestyle changes and concerns about weight gain.
Can endometriosis cause cancer?
Can endometriosis cause cancer is a really common concern that research has been addressing. There seems to be a very small associated increased risk of ovarian, breast and thyroid cancer, but this risk is exceptionally small when you compare it to the risk of these cancers in the general population.
Surgical treatment to remove all the endometriosis that can be seen on ovaries, can reduce the risk of ovarian cancer.
Currently, guidelines state that people with endometriosis can be reassured about cancer risk and not to worry. European guidelines recommend that women with endometriosis should concentrate on reducing cancer risks – aka eat healthily, avoid sunbeds, stop smoking, exercise and maintain a healthy weight – which is the same advice given to the general population.
What are the bowel symptoms of endometriosis?
The bowel symptoms of endometriosis can be very similar to irritable bowel syndrome. These include bloating, constipation, diarrhoea or abdominal pain that can change throughout your menstrual cycle. However, some symptoms are more typical for endometriosis especially if you also have very painful periods. These include deep pain inside your pelvis during sex, pain on opening your bowels in your rectum or anus or even bleeding when you open your bowels. These are mostly felt during your period, but you may experience them throughout the month.
What are the long-term complications or effects of untreated endometriosis?
Endometriosis can cause heavy or prolonged bleeding, if untreated, this can lead to anaemia and symptoms of dizziness, fatigue and shortness of breath. Untreated endometriosis can cause chronic pain which can affect your quality of life. Untreated endometriosis may reduce fertility if left untreated, but fertility treatment can often help you get pregnant. We should never forget the impact of endometriosis and its symptoms on your mental health, relationships, working life and sexual wellbeing – which for many people are the most longstanding features when dealing with the condition for a long time.
Endometriosis treatment FAQs
How can you help endometriosis pain?
Endometriosis can be one of the most severe pains you will experience. You can concentrate on one way to help, or many different ways added together which often results in better overall relief.
Treatment options include:
- Simple painkillers (ie paracetamol and ibuprofen) are a good place to start, but may not fully help. Stronger painkillers are available from your doctor such as strong anti-inflammatories. Medications such as mefenamic acid and tranexamic acid can help with heavy bleeding alongside pain.
- Hormonal treatment is a very effective treatment for symptoms. This can include hormonal contraceptives (which can be prescribed by your GP), or hormonal injections to turn off your menstrual cycle called gonadotrophin releasing hormone agonists (these are only available from hospital specialists). One of the most effective hormonal contraceptives for endometriosis is the hormonal coil, but this blog can help you choose the best contraceptive for endometriosis, by discussing all the pros and cons.
- Surgical procedures are an important treatment for endo where endometrial deposits in the pelvis can be cut or burned away and any scar tissue that has formed can be removed.
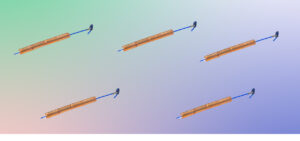
- Simple non-invasive gadgets, such as a TENS machine (our favourite is Myoovi) can be used alongside painkillers, are non-invasive and have few side effects but can be expensive to purchase…(The Lowdown has a discount link available!)
- The humble hot water bottle is one of our community’s favourites!
- Pelvic physiotherapy is an incredible way to ease pain…seriously they are like magicians…and many women’s health physios, including our fabulous Kathryn, have specialist interests in endometriosis.
- Supplements can be beneficial, and the nutrients found in complexes such as Wild Nutrition’s Endo Support can help overcome symptoms such as tiredness and fatigue.
- Complementary therapies – never underestimate the power of a healthy lifestyle, diet and exercise for helping to relieve pain and improve your mood. Some women also find treatments including acupuncture, reflexology and homeopathy helpful
What contraception is best for endometriosis?
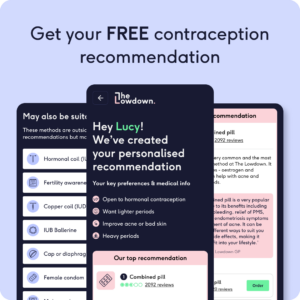
Hormonal contraceptives are an important part of treatment for endometriosis. The best contraception for endometriosis is the one that suits you the best. Research shows that hormonal contraceptives can reduce pain and symptoms from endo, but you also need to balance their use against any side effects and your medical history. We have taken a deep dive into this in our blog about the best contraceptive for endometriosis. A really excellent place to start deciding, would be using our contraception recommender which can suggest options that are safe for you and help with your symptoms.
Are there any natural treatments for endometriosis?
There are many natural treatments for endometriosis and we know from research that at least 70% of endo sufferers use alternative therapies to help their symptoms. However, research doesn’t yet help us much to decide which natural treatments are best and more of it needs to be done! Some studies suggest that exercise, physiotherapy and acupuncture can be useful for women with endometriosis – and we think it’s definitely worth a try.
Studies suggest that diet and nutrition plays a role in endometriosis and symptoms, but there’s no clear evidence from them yet. We do know that vitamin D supplementation may help as well as ensuring you have a good intake of unsaturated fats, omega-3 and fibre.
Overall, maintaining a healthy body and mind is exceptionally important when dealing with a chronic condition like endometriosis, and if any natural treatments can help you with this, go for it.
What is endometriosis surgery?
Endometriosis surgery is when a surgical procedure is used to remove endometrial deposits from inside the pelvis. The type of surgery is usually a laparoscopy which is the medical term for a camera procedure or key hole surgery. A diagnostic laparoscopy is when a camera is inserted through a small incision in your abdomen into the pelvis to look for the signs of endometriosis and give a diagnosis. During this procedure, you will be under a general anaesthetic. While this procedure is to provide a diagnosis, you can also have treatment for endometriosis at the same time.
Types of surgical treatment of endometriosis:
- Ablation surgery is where endometrial deposits are burned away.
- Excision surgery is where endometrial deposits are cut away. Research suggests that excision surgery is a better option than ablation to reduce endometriosis associated pain, especially for deep endometriosis. However, excision surgery for deep endometriosis should be performed in a centre of expertise.
- Cystectomy surgery removes ovarian cysts caused by endometriosis which are called endometriomas or chocolate cysts. Cystectomy is preferred to treat ovarian cysts rather than draining them, as they are less likely to return if you remove them completely.
- Nerve surgery includes either ablation or removal of certain nerves in the pelvis with the aim to improve endometriosis associated pain. Ablation of the nerves is not recommended as it doesn’t seem to improve pain any more than removing the endometrial deposits alone. Removal of the nerves could improve pain but only when an expert performs the procedure and there may be long term complications such as constipation and urinary urgency.
- Hysterectomy is the removal of the womb and is not a standard treatment for endometriosis. Hysterectomy may sometimes be performed as part of a larger operation to remove deep endometriosis or alongside removing parts of the bowel.
Can endometriosis grow back after surgery?
Endometriosis can recur after surgical treatment. The rates of recurrence vary massively in research studies from between 0% to 89%….which isn’t particularly helpful. It’s hard to predict who will have recurrence of their symptoms after surgery, but research suggests that recurrence is more common if you have surgery at a younger age, have a strong family history of endometriosis or have adhesions (scar tissue) seen during the procedure. European endometriosis guidelines recommend that after surgery, hormonal treatment with the combined pill or hormonal coil should be offered for 18 to 24 months to prevent endometriosis associated period pain from recurring.
How can I find a specialist in endometriosis?
At The Lowdown, we strongly believe that everyone should be entitled to the same level of treatment and care.
Everyone in the UK has access to free treatment on the NHS and this should be equitable and of the same quality. The NHS has accredited endometriosis centres, you can find your nearest using this website. If you are unhappy with the treatment you are currently receiving, you have a right to ask for a second opinion, and you have a right to choose where you are referred to for specialist treatment.
If you are elsewhere in the world and your healthcare is insurance based – check to see what is covered. Even if you are not able to access a laparoscopy, you can still access treatment using hormonal contraceptives and medications which are more readily available.
Do I need treatment or can endometriosis stop developing and not grow further?
Endometriosis is a mysterious disease. We still don’t fully know the cause, although there are theories. We know that in some people, endometriosis can stop developing and even regress. We do not know how to predict whose condition will regress or stop or how long it will take. However, if endometriosis is allowed to become severe it can cause debilitating and painful symptoms and have long term effects and impact fertility, so you may want to consider treatment rather than waiting to see what happens.
Tags
- ESHRE Endometriosis Guideline 2022.
- Meuleman C, Vandenabeele B, Fieuws S, Spiessens C, Timmerman D, D’Hooghe T. High prevalence of endometriosis in infertile women with normal ovulation and normospermic partners. Fertil Steril 2009;92: 68-74.
- Endometriosis UK: Endometriosis, Fertility and Pregnancy 2023.
- Armour M, Sinclair J, Chalmers KJ, Smith CA. Self-management strategies amongst Australian women with endometriosis: a national online survey. BMC Complement Altern Med. 2019 Jan 15;19(1):17.
One of The Lowdown’s fab Clinical Directors, Dr Frances Yarlett MBBCh (Hons) BSc (Hons) MRCP (2016) MRCGP DFSRH completed her medical training from Cardiff University in 2013. She is currently working as a salaried GP partner in Sheffield with an interest in complex medical patients and women’s health. Fran is really passionate about patient choice and wants to empower women to take control of their bodies and contraception needs.